ABSTRACT
OBJECTIVES: to assess the prevalence of maternal gestational anemia and its association with the birth weight.
METHODS: retrospective longitudinal observational study in a cohort of 370 pregnant women. Anthropometric, biochemical, ginecobstetric and sociodemographic data of both mothers and newborns were evaluated. The results of maternal erythrocyte indices were analyzed and contrasted with newborns anthropometrical data.
RESULTS: the mean age of the pregnant women was 27±6 years, with a mean gestational age of 32±6 weeks at the assessment moment, 56.2% were overweight. The prevalence of anemia was 28.6%. 47.2% women with anemia and 36% women without anemia had low birth weight/very low birth weight newborns (p=0.009). Of the children born to mothers with iron deficiency anemia, 20% had low birth weight and 15% very low birth weight. 54.3% newborns with global undernutrition or at risk of developing it were born to women with underweight(p=0.046), in addition, the higher the maternal weight, the lower the number of term newborns with risk of short height (p<0.001).
CONCLUSIONS: there is relationship between the anemia, the maternal nutritional status and the birth weight.
Keywords:
Anemia, Birth weight, Pregnancy, Maternal nutrition
RESUMO
OBJETIVOS: evaluar la prevalencia de anemia gestacional materna y su relación con el peso al nacer.
MÉTODOS: estudio observacional longitudinal retrospectivo en una cohorte 370 mujeres gestantes. Se evaluaron variables demográficas clínicas y antropométricas tanto de las madres como de los recién nacidos. Se analizaron los resultados de los índices eritrocitarios maternos y se contrastaron con los datos antropométricos de los neonatos.
RESULTADOS: la edad promedio de las gestantes fue de 27±6 años con edad gestacional promedio al momento de la evaluación nutricional de 32±6 semanas, el 56,2% presentaron exceso de peso. La prevalencia de anemia fue de 28,6%. El 47,2% de gestantes con anemia y el 36% de gestantes sin anemia tuvieron neonatos con bajo peso/muy bajo al nacer (p=0,009). De los niños nacidos de madres con anemia ferropénica 20% tuvo bajo peso y 15% muy bajo peso al nacer. El 54,3% de neonatos con desnutrición global o en riesgo de desarrollarla fueron hijos de madres con bajo peso (p=0,046), además a mayor peso materno, menor cantidad de neonatos a término con riesgo de baja talla (p<0,001).
CONCLUSIONES: existe relación entre la anemia, el estado nutricional materno y el peso al nacer.
Palavras-chave:
Anemia, Peso al nacer, Gestación, Nutrición materna
IntroductionAnemia represents one of the main affectations at hematological level among women of reproductive age and pregnant women. In Colombia, to the year 2015 the anemia prevalence in pregnancy was 26.2% and the iron deficiency anemia represented 59.2%;
1 while at the departmental level for the year 2019 a prevalence 48.4% of anemia was reported in the evaluated women.
2Its most common causes are blood loss, insufficient production of red blood cells or excessive destruction of them;
3 during pregnancy, anemia is part of a physiological adaptive process caused by changes in the blood volume that result in a consequent hemodilution. However, anemia can be caused by factors such as acute infections, chronic inflammation, hemoglobinopathies and nutrient deficiencies such as folate, vitamin B12 and iron.
4The latter is one of the main nutrients of interest in pregnancy, since it participates on the transfer of oxygen through maternal-placental tissues, especially to meet the high brain demands of the fetus, and it also plays an important role in numerous enzymatic processes, so its needs tend to increase from the second trimester of pregnancy to support fetal metabolic needs and for formation on the reserve that will support its needs during the first 6 months of life.
5-6When anemia occurs or is maintained during pregnancy, it has major implications for the mother-child relationship; it has been reported that insufficient hemoglobin levels can limit the fetal oxygen availability, causing intrauterine growth restriction and directly affecting birth weight.
7 This has been explained by Barker's theory, indicating that the fetus can make numerous metabolic adaptations such as optimizing the supply of maternal nutrients to ensure its survival, impacting its growth and development.
8-9This may represent negative consequences at the fetal level, taking into account that iron deficiency has been reported to trigger decreased motor, neurophysiological and cognitive development in children,
10 leading to social, economic and health limitations during adulthood such as chronic non-communicable diseases, impacting on human capital.
Recent studies have evaluated the effect of anemia during pregnancy and perinatal outcomes, including birth weight, such as that carried out in 211 full-term newborns in northwestern Ethiopia, in which a prevalence of 29% was found of low birth weight in the newborns of mothers with anemia, in addition to the fact that newborns of anemic mothers were 3.51 times more likely to have low birth weight compared with non-anemic mothers with, where socioeconomic factors such as the mother's educational level were significant variables associated with low birth weight.
11 This coincides with a recent study conducted in adult pregnant women in Bolívar, Colombia, in which it was found that birth weight was inversely associated with maternal hemoglobin levels, and that gestational anemia was positively associated with sociodemographic conditions related to poverty.
12The aim of this study was to evaluate the prevalence of maternal gestational anemia and its relationship with birth weight, since there are few studies carried out at the local level that address this problem, and thus identify its impact on fetal outcomes, specifically on birth weight.
MethodsA retrospective a longitudinal observational study was carried out in a cohort of pregnant women between 2018 and 2020 at the San Vicente Fundación Hospital (HSVF), Medellín-Colombia. The selected population was 901 pregnant women of legal age in all trimesters on pregnancy, who were registered in the database of nutritional screening carried out on said population during the mentioned years and who, in addition, had sociodemographic, biochemical, clinic data and with the anthropometry of the newborn included in the study.
Exclusion criteria were fetal death, twin or multiple pregnancy, pregnant women in intensive care, and pregnant women or neonates with incomplete data. A total of 531 pregnant women who did not meet the eligibility criteria were excluded, studying a convenience sample of 370 pregnant women.
Among the study variables the following were considered:
- Sociodemographic variables: characteristics such as type of health affiliation (contributory, subsidized), marital status (single, married, common-law union), age of the mother, and level of education were taken, which were extracted from the medical history on the patients registered in the SAP application.
- Clinical variables: the admission diagnosis for which the mother was attended within the HSVF, the woman's parity, gestational age at the time of nutritional screening, and the type of delivery were considered.
- Maternal anthropometric variables: weight and height were taken from the data recorded in the nutritional screening of the pregnant woman, completed by the HSVF dietician nutritionists. With these data, the gestational body mass index (BMI) was calculated. This indicator was classified according to cut-off points of Atalah and Castillo (underweight, normal, overweight and obesity). 13
- Anthropometric variables of the newborn: the weight and length at birth obtained from the recollection in the medical records of the babies born in the HSVF during the mentioned periods, or through telephone calls to the mothers whose babies were born in other hospitals were taken. The indicators weight/length, weight/age and length/age in the full-term neonates were calculated and classified based on resolution 2465 of 201614; Z-scores were calculated in the WHO Anthro software. For preterm neonates, the indicators of weight for age and length for age were classified according to the cut-off points according to Fenton,15 for which the Peditools program was used.
- Biochemical variables: maternal data of hemoglobin (Hb), hematocrit (HCT), mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH) and mean corpuscular hemoglobin concentration (MCHC) were taken from the laboratory results available in the medial records, corresponding to the hospitalization in which the pregnant woman received the nutritional screening.
- Hemoglobin was corrected according to the height at sea level of Medellín (1500 m), and the WHO correction cut-off points were used. 16 Corrected hemoglobin was used to diagnose anemia in pregnancy, defining anemia as an Hb level <11.0 mg/dL in the first and third trimester, and <10.5 mg/dL in the second trimester of the pregnancy. 17 In addition, the severity of anemia was defined according to WHO cut-off points. 18
- MCV and MCH were used to define the type of anemia, defining hypochromia at MCH values <28.2 pg in the first and second trimester and <27.5 pg in the third trimester, hyperchromia at MCH values >30.8 pg in the first and second trimester and >30.7 pg in the third trimester, and normochromia at MCH values between these ranges19; and normocytic, macrocytic and microcytic anemia at MCV values between 80 and 100 fl, >100 fl and <80 fl, respectively.20
The recollected information was consolidated in an Excel file and later processed and analyzed in the statistical package SPSS V.24.
The qualitative variables are described according to absolute number and percentage, the quantitative variables according to the median and interquartile range (p
25-p
75) since they did not follow the assumption of normal distribution.
Differences in the anthropometric variables of the newborn were searched, stratifying by type of delivery (full-term, preterm) according to presence or absence of gestational anemia, severity of anemia (mild, moderate and severe) and type of anemia. We evaluated whether there were differences in the birth weight and BMI according to presence or absence of gestational anemia. For the contrast of hypothesis between qualitative variables, the Pearson Chi Square test was used, for the contrast of hypothesis between quantitative variables and dichotomous qualitative variables, the Mann Whitney U test was used, for the comparison between numeric variables and polytomous qualitative varibles the Kruskal Wallis test was used. A value of
p<0.05 was considered significant
. The ORs with their respective CI95% were calculated to assess the relationship between the presence of maternal anemia with birth weight, type of delivery and the individual anthropometric indicators of the newborn.
For the execution of this study, we had the endorsement of the Research Directorate and the Ethics Committee of the
San Vicente Fundación Hospital, this study is considered without risk since data were taken from medical records and the nutritional screening database.
ResultsThe sociodemographic, anthropometric, biochemical and clinic characteristics of the mothers are described in Table 1. The mean age of the pregnant women was 27 ± 6 years. The gestational age at the time of the nutritional assessment was 32 ± 6 weeks, the majority were in their third trimester of pregnancy at the moment of the nutritional screening (86.6%) and the 35.9% were primiparous.
Regarding the educational level of the pregnant women, more than half had only primary or secondary education (24.9% and 29.2% respectively), while 16.2% did not refer any educational level. 50.5% belonged to contributive regimen in their health affiliation, and the half lived in common-law union (53.5%).
The most frequent admission diagnoses were threatened preterm delivery, labor, premature rupture of membranes, maternal heart disease and other diseases of the circulatory system. Regarding the type of delivery, 62.2% has a history of delivery by caesarean section.
Regarding maternal nutritional status, more than half had some type of excess weight, while 15.9% were underweight. A prevalence of anemia of 28.6% was found (106 of pregnant women studied) (Table 1).
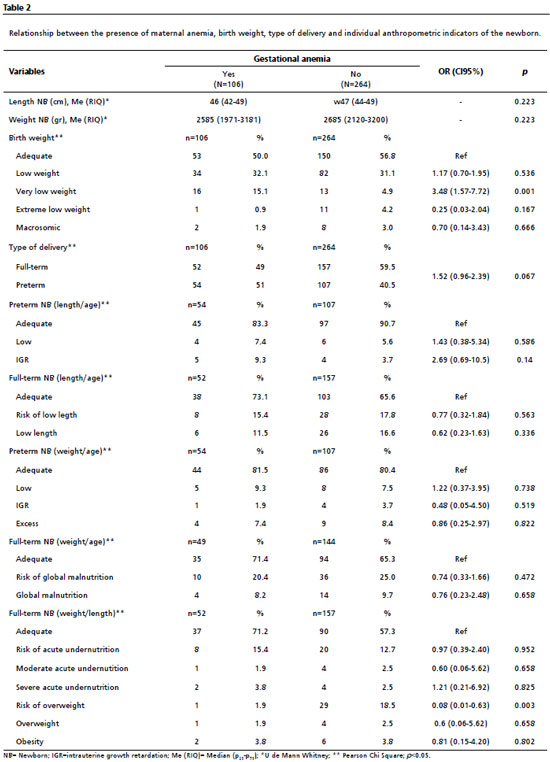
Maternal anemia and nutritional status of the newbornTable 2 shows the relationship between the presence of maternal anemia, birth weight, type of delivery and the individual anthropometric indicators of the neonate. All newborns had an adequate mean weight and length. 50% of pregnant women with anemia had newborns with adequate weight and 47.2% were neonates with low weight and very low birth weight, these percentages differ from those observed in pregnant women without anemia, who had 56,8% neonates with adequate weight and 36% with low weight and very low birth weight. An association was found between very low birth weight and the presence of gestational anemia (OR= 3.48; CI95%=1.57-7.72). There was no significant difference between the presence of anemia and the individual indicators of length/age, weight/age and weight/length or the type of delivery.
The type of maternal anemia and its relationship with the birth weight and the type of delivery are shown in Table 3. Most of the newborns of pregnant women who presented normochromic normocytic anemia had an adequate birth weight; 35% of the children born to mothers with iron deficiency anemia had low or very low birth weight. There was statistically significant difference between the type of anemia and birth weight (
p=0.045). The number of preterm neonates born to mothers with anemia was greater, although there was no significant difference.
Regarding the severity of maternal anemia and the individual neonatal anthropometric indicators, no significant differences were found between the studied variables. The mean of weight and length at birth were adequate, 54.5% of the full-term newborns of mothers with moderate anemia presented low length or risk to presenting it, and 20.5% of the full-term newborns of mothers with mild anemia were below -1SD in the weight to length indicator.
Maternal nutritional status, neonatal anthropometry and birth weightTable 4 shows the differences between maternal nutritional status, individual neonatal anthropometric indicators and birth weight. It was found that the higher the maternal weight, the lower the number of full-term newborns with risk of low length (
p<0.001). Regarding the weight for age indicator in full-term newborns, the highest percentage of pregnant women classified as underweight at the time of the nutritional screening had newborns with global malnutrition (20%) or risk to developing it (34.3%), with significant differences (
p=0.046). There was a directly proportional trend between birth weight and maternal weight, with the exception of obese pregnant women; there was a higher proportion of newborns with low birth weight and very low birth weight in overweight pregnant women, compared to those underweight or normal weight.
Table 5 shows the relationship between birth weight, maternal anthropometry and the presence of maternal anemia. 14.3% of the newborns of mothers with anemia had inadequate weight due to deficit or excess; 32.4% of newborns with low weight and 12.5% of newborns with very low weight were children of mothers with anemia who were underweight at the time of the nutritional screening, while a lower percentage (14.6% of newborns with low weight and 7.7% of those born with very low weight) were children of mothers without anemia who were underweight.
DiscussionThe prevalence of anemia and its relationship with low birth weight in pregnant women who underwent nutritional screening were evaluated. The findings of this study indicate a high prevalence of anemia in the studied population, as well as a higher proportion of maternal anemia in neonates with low birth weight, and the maternal nutritional status is associated with the length/age and weight/age indicators in the full-term newborns.
The presence of anemia in the pregnant women of this study coincides with the finding at the national level in the National Survey of the Nutritional Situation-ENSIN 2015, in which a prevalence of anemia of 26.2% was found in the pregnant women evaluated,
1 and it was lower than the findings of the Food and Nutritional Profile of Antioquia (PANA) 2019, which found a prevalence of anemia in the 48.4% of adult and adolescent pregnant women surveyed,
2 which may possibly be due to the favorable sociodemographic characteristic found in the present cohort in comparison with the characteristics of the evaluated population in the Antioquia study, taking into account that in the latter Medellín city was not included in the sample.
Despite this, the previous results were similar to the findings of the study by Madrid-Pérez
et al. ,
21 in which they determined the relationship between maternal hemoglobin per trimester of pregnancy and birth weight in 474 prenatal medical records from 9 health centers in Antioquia, they found a statistically significant association between maternal hemoglobin in the third trimester and birth weight (BW) by categories (BW<3,000g y BW between 3,000g-4,000g).
21Likewise, Restrepo-Mesa
et al. ,
22 determined the association between maternal BMI and hemoglobin concentration with birth weight from 336 medical records of pregnant women whose prenatal controls and deliveries had taken place in some of the 7 clinical unities of the Medellín network, finding that the gestational BMI was associated with BW where a lower birth weight was more prevalent in underweight women.
22 These findings differ from our study, where no statistically significant difference was found between the gestational BMI and BW, this may be due to the presence of other health conditions that could influence in the weight of the newborns regardless of maternal weight.
Neither were significant differences found between the presence of anemia and the individual indicators of length/age, weight/age and weight/length, this results contrast with those described by Sá
et al. ,
23 in a study carried out on 54 Brazilian pregnant women classified as at risk of low socioeconomic level in which the frequency of gestational anemia was evaluated and its relationship with the nutritional status of the full-term newborn finding that, despite the high frequency of maternal anemia, the maternal nutritional status was not associated with the development of anemia or the birth weight.
23A higher number of preterm neonates born to mothers with anemia was observed, although there was no significant difference. This finding indicates that there could be a relationship between maternal anemia and preterm birth, however, the low number of patients in the analyses could explain why no statistical differences were found.
There was heterogeneity in the findings of variables such as severity of anemia, which can be explained by the difference in the proportion on women with mild, moderate or severe anemia, resulting in groups that were not very comparable to each other.
It should be noted that a large number of neonates with low birth weight were born to mothers with iron deficiency anemia, currently representing a public health problem at national level if contrasted with national findings, where 59.2% of pregnant women surveyed presented iron deficiency anemia.
1 Numerous authors have found that the most of women do not receive the necessary amounts of iron during pregnancy, which not only implies greater risk for the mother: perinatal infection, preeclampsia, bleeding and behavior impairment, but also higher morbidity and fetal death.
24Our study is one of the few carried out in our environment that have evaluated the relationship between maternal anemia seen as type and severity of anemia, and its relationship with birth weight taking into account individual indicators of neonatal anthropometry. As limitations of the study, this was a retrospective study of secondary sources, and in many cases the mother's memory had to be used to recollect some anthropometric data. In addition, not all screened mother had the measure of erythrocyte markers, so they were excluded from the study.
In conclusion, there was relationship between the anemia and maternal nutritional status and birth weight. Despite the fact that most of the newborns had an adequate birth weight in both pregnant women with and without anemia, the prevalence of low weight and very low birth weight is worrying due to the high number of reported cases, which reflects the need of strengthen public policies and food security, rescuing the local food culture and access to food produced in the region, as well as the creation of micronutrients supplementation strategies, monitoring the intake and maternal weight gain that favor and have a positive impact at an adequate birth weight. Additionally, the present findings represent an important starting point to reinforce the nutritional attention for the pregnant population of the department through multidisciplinary work.
Future studies are recommended to evaluate the relationship between maternal anemia seen from its type and severity, and the birth weight of neonates in different contexts, and thus be able to determinate the impact of current interventions in public health.
References1. Instituto Colombiano de Bienestar Familiar (ICBF). Instituto Nacional de Salud. ENSIN: Encuesta Nacional de Situación Nutricional 2015. [access in 2022 Oct 10]. Available from:
https://www.icbf.gov.co/bienestar/nutricion/encuesta-nacional-situacion-nutricional#ensin32. Universidad de Antioquia, MANÁ, Gobernación de Antioquia. Perfil Alimentario y Nutricional de Antioquia; 2019. [access in 2022 Oct 10]. Available from:
https://www.udea.edu.co/wps/wcm/connect/udea/ba8c4eac-c8ad-43aa-9a6f-7f9f143d28a0/resumen_ejecutivo_perfil_alimentario_FINAL.pdf?MOD=AJPERES&CVID=n3658bG3. Braunstein E. Introducción a la anemia. Trastornos de la sangre-Manual MSD versión para público general [
Internet]. 2021. [access in 2022 Oct 10]. Available from:
https://www.msdmanuals.com/es-co/hogar/trastornos-de-la-sangre/anemia/introducción-a-la-anemia4. Friel L. Anemia en el embarazo. Ginecología y obstetricia-Manual MSD versión para profesionales [
Internet]. 2021. [access in 2022 Oct 10]. Available from:
https://www.msdmanuals.com/es-co/professional/ginecología-y-obstetricia/complicaciones-no-obstétricas-durante-el-embarazo/anemia-en-el-embarazo.5. Marangoni F, Cetin I, Verduci E, Canzone G, Giovannini M, Scollo P,
et al. Maternal diet and nutrient requirements in pregnancy and breastfeeding. An Italian consensus document. Nutrients. 2016 Oct; 8 (10): 629.
6. Means RT. Iron deficiency and iron deficiency anemia: Implications and impact in pregnancy, fetal development, and early childhood parameters. Nutrients. 2020 Feb; 12 (2): 447.
7. Figueiredo ACMG, Gomes-Filho IS, Silva RB, Pereira PPS, Da Mata FAF, Lyrio AO,
et al. Maternal anemia and low birth weight: A systematic review and meta-analysis. Nutrients. 2018 May;10 (5): 601.
8. Rodríguez Vargas N, Martínez Pérez TP, Martínez García R, Garriga Reyes M, Fernández-Britto JE, Martínez Fure G. Programación in utero: un desafío. Rev Cuba Invest Bioméd. 2014; 33 (1): 94-101.
9. Hernández-Triana M. Poor management of low birth weight compounds obesity and chronic diseases in Cuba. MEDICC Rev. 2015 Apr; 17 (2): 44-7.
10. Gonzales-Medina C, Arango-Ochante P. Resultados perinatales de la anemia en la gestación. Rev Peru Ginecol Obstet. 2019; 65 (4): 519-26.
11. Engidaw MT, Eyayu T, Tiruneh T. The effect of maternal anaemia on low birth weight among newborns in Northwest Ethiopia. Sci Rep. 2022 Sep; 12 (1): 15280.
12. Puerto A, Trojan A, Alvis-Zakzuk NR, López-Saleme R, Edna-Estrada F, Alvarez A,
et al. Iron status in late pregnancy is inversely associated with birth weight in Colombia. Public Health Nutr. 2021; 24 (15): 5090-100.
13. Atalah E, Castillo C, Castro R. Propuesta de un nuevo estándar de evaluación nutricional en embarazadas. Rev Med Chile. 1997; 25: 1429-35.
14. Ministerio de Salud y Protección Social (Colombia). Resolución Número 2465 de 14 Jun 2016. Por la cual se adoptan los indicadores antropométricos, patrones de referencia y puntos de corte para la clasificación antropométrica del estado nutricional de niñas, niños y adolescentes menores de 18 años de edad, adultos de 18 a 64 años de edad y gestantes adultas y se dictan otras disposiciones. [
Internet]. Colombia: Ministerio de Salud y Protección Social; 2016. [access in 2022 Oct 10]. Available from:
https://www.icbf.gov.co/sites/default/files/resolucion_no. _2465_del_14_de_junio_de_2016.pdf15. Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013 Apr; 13 (1): 59.
16. Organización Mundial de la Salud (OMS). Concentraciones de hemoglobina para diagnosticar la anemia y evaluar su gravedad [
Internet]. 2011. [access in 2022 Oct 10]. Available from:
http://www.who.int/vmnis/indicators/haemoglobin_es.pdf17. Api O, Breyman C, Çetiner M, Demir C, Ecder T. Diagnosis and treatment of iron deficiency anemia during pregnancy and the postpartum period: Iron deficiency anemia working group consensus report. Turk J Obstet Gynecol. 2015; 12 (3): 173-81.
18. Goonewardene M, Shehata M, Hamad A. Anemia in pregnancy. Best Pract Res Clin Obstet Gynaecol. 2012; 26 (1): 3-24.
19. Canalejo K, Tentoni J, Aixalá M, Jelen AM. Valores de referencia del hemograma en embarazadas, con tecnología actual. Bioq Patol Clín. 2007; 71 (2): 52-4.
20. Carrillo P, Garcia A, Soto M, Rodriguez G, Pérez J, Martinez D. Cambios fisiológicos durante el embarazo normal. Rev Fac Med UNAM. 2021; 64: 39-48.
21. Madrid Pérez C, Restrepo Mesa S, Aristizabal Tirado J. Relación de la hemoglobina materna y el peso al nacer en Antioquia-Colombia. Rev Bras Saúde Matern Infant. 2021; 21 (1): 197-205.
22. Restrepo Mesa SL, Parra Sosa BE, Arias Gómez J, Zapata López N, Giraldo Díaz CA, Restrepo Moreno CM,
et al. Estado nutricional materno y su relación con el peso al nacer del neonato, estudio en mujeres gestantes de la red pública hospitalaria de Medellín, Colombia. Persp Nutr Hum. 2012; 14 (2): 199-208.
23. Sá SA, Willner E, Pereira TAD, Souza VR, Boaventura GT, Azeredo VB. Anemia in pregnancy: Impact on weight and in the development of anemia in newborn. Nutr Hosp. 2015 Nov; 32 (5): 2071-9.
24. Abu-Ouf NM, Jan MM. The impact of maternal iron deficiency and iron deficiency anemia on child's health. Saudi Med J. 2015; 36 (2): 146-9.
Received on May 15, 2023
Final version presented on May 18, 2023
Approved on June 27, 2023
Associated Editor: Aurélio Costa
Authors contributions: Correa-Mesa IC and Montoya-Montoya S participated in the conceptualization and design of the study. Correa-Mesa IC extracted the information from the medical records. Villada-Ochoa OA performed the statistical analysis. All the authors contributed to data synthesis, writing and final revisions of the manuscript. The authors approved the final version of the article and declare no conflict of interest.
 ; Susana Montoya Montoya2
; Susana Montoya Montoya2 ; Oscar Alonso Villada Ochoa3
; Oscar Alonso Villada Ochoa3