ABSTRACT
OBJECTIVES: to analyze the factors associated with the risk of developmental delay in children under five years of age hospitalized for primary care-sensitive conditions.
METHODS: a quantitative, cross-sectional study conducted with 90 children under five years old and their family caregivers. The risk of developmental delay was assessed using the Survey of Well-Being of Young Children (SWYC). Associations between variables were analyzed using Poisson regression with robust variance, supported by SPSS software, version 21.0.
RESULTS: the risk of developmental delay was identified in 22.2% of the children and was associated with low birth weight (PR = 1.17), behavioral problems (PR = 1.14), mothers with two children (PR = 1.18), and living in areas without basic sanitation (PR = 1.19).
CONCLUSION: the risk of developmental delay was positively associated with child-related factors (low birth weight), caregiver characteristics (mother with two children), and environmental conditions (lack of basic sanitation). Monitoring of child development should be integrated into all levels of child and family healthcare, aiming at comprehensive development, especially in vulnerable contexts. Public policies and actions must address the social determinants of health that influence care in both primary healthcare and hospital services.
Keywords:
Child development, Ambulatory care sensitive conditions, Hospitalized child, Child health, Child behavior
RESUMO
OBJETIVOS: analisar os fatores associados ao risco de atraso no desenvolvimento infantil de crianças menores de cinco anos internadas por condições sensíveis à atenção primária.
MÉTODOS: estudo quantitativo, transversal, realizado com 90 crianças menores de cinco anos e seus cuidadores familiares. O risco de atraso no desenvolvimento infantil foi avaliado por meio do Survey of Well-Being of Young Children (SWYC). A associação entre as variáveis foi analisada por regressão de Poisson com variância robusta, utilizando o software SPSS, versão 21.0.
RESULTADOS: o risco de atraso no desenvolvimento infantil foi identificado em 22,2% das crianças e apresentou associação com baixo peso ao nascer (RP = 1,17), alterações de comportamento infantil (RP = 1,14), mãe com dois filhos (RP = 1,18) e residência em local sem saneamento básico (RP = 1,19).
CONCLUSÃO: o risco de atraso no desenvolvimento infantil esteve positivamente associado a variáveis relacionadas à criança (baixo peso ao nascer), ao cuidador (mãe com dois filhos) e ao ambiente (ausência de saneamento básico). A vigilância do desenvolvimento infantil deve ser incorporada a todos os níveis de atenção à saúde da criança e da família, com foco no desenvolvimento pleno, especialmente em contextos de vulnerabilidade. Ações e políticas públicas devem considerar os determinantes sociais da saúde que impactam o cuidado na atenção primária e nos serviços hospitalares.
Palavras-chave:
Desenvolvimento infantil, Condições sensíveis à atenção primária, Criança hospitalizada, Saúde da criança, Comportamento infantil
IntroductionChild Development (CD) is a dynamic, progressive and continuous process, which encompasses physical, cognitive, socioemotional, linguistic and behavioral aspects.
1 The success in achieving it depends on the interaction with the environment in which children is located, as well as the social relationships they build.
2,3 CD is particularly sensitive during the early childhood, when the brain is in its maximum activity and more vulnerable to external influences. This stage involves the formation of the individual's affective and emotional foundation, in addition to the development of brain areas crucial for personality, character, learning ability and memory.
1It is estimated that approximately 250 million children under five years of age, living in low- and middle-income countries, will not reach their full potential. This represents a four-fold increased risk of developmental delay compared to high-income countries, with an overall prevalence of 22.5% of children with suspected delay.
3In Brazil, the estimated prevalence of suspected CD is 12%,
4. This is associated with factors such as poor infant stimulation, unsafe environments (e.g., domestic violence), low maternal and paternal education levels, maternal depression, prematurity, lack of safe drinking water and basic sanitation, low birth weight and infant anemia.
4-7 The crucial influence of environment on child development
1 raises concerns about the potential risk for CD when children are hospitalized, particularly by avoidable causes, such as in hospitalizations due to primary care-sensitive conditions (ICSAP – Portuguese acronym).
Primary care-sensitive conditions (PCSC) are a group of diseases and health problems that should not result in hospitalization, if Primary Healthcare (APS – Portuguese acronym) actions are effectively implemented. The Brazilian ICSAP List demonstrates groups of causes of hospitalizations and diagnoses, such as vaccine-preventable diseases and respiratory, infectious, cardiovascular, endocrine and neurological diseases. The presence of ICSAPs functions as one of the manners to measure the assistance efficacy and effectiveness provided by the APS.
8 Hospitalizations in early childhood may represent an additional barrier to the full development of children. Being isolated in a hospital room may hinder children's motor skills, as well as suppress the expression of creativity and autonomy in the relationships with their peers and family.
8-10The World Health Organization (WHO) defines the Social Determinants of Health (SDOH) as the conditions in which people live and work.
11 For the National Commission on Social Determinants of Health (CNDSS – Portuguese acronym), the SDOHs imply in the process health-disease of the population in the social, economic, cultural, ethnic or racial, psychological and behavioral areas.
11 For children to achieve their full development, it is necessary to consider the direct relationship with the environment where they live, as well as their continuous interaction over time.
12 Being exposed to precarious socioeconomic conditions, economic instability and lack of public awareness generate unhealthy environments for children.
13Since they are causes of hospitalizations that would be avoidable if assisted by APS, the professionals that act in this level of care may contribute to its prevention. In the hospital care level, educational practices may be directed to guide caregivers towards the measures that can be adopted in the CD promotion, as well as in the prevention of recurrent ICSAPs.
12,14,15For the elaboration of educational practices in the healthcare area, focusing on mitigating further hospitalizations and contributing to CD of children hospitalized due to PCSC, it is necessary, initially, to identify factors associated with these events. The objective of this study was to analyze factors associated with the risk of delay in the development of children under five years of age hospitalized due to PCSC.
MethodsThis was a cross-sectional quantitative study, conducted in a philanthropic hospital in Recife, Pernambuco, a leading institution for both North and Northeast regions in child healthcare. The pediatric ward was selected due to the prevalence of PCSC in this department.
The sample was composed of children hospitalized due to PCSC and their respective caregivers. Caregivers from the family (and their respective children) who provided care for less than 20 hours per week were excluded from the sample. Sampling was non-probabilistic, based on convenience.
Sample size calculation was performed for a finite population, considering a 95% confidence interval, 5% margin of error, population size of 128 individuals (considering the ICSAPs in the first four months of 2020) and a frequency of risk of delay in child development (CD) of 27.5%.
16 From this calculation, we defined a minimum sample of 90 participants.
Data collection occurred from April to August 2022, using a semi structured form to register socioeconomic and demographic variables. The risk for CD delay was assessed by means of the Survey of Well-being of Young Children – Brazilian Version (SWYC-BR), an screening tool for changes in development and behavior of children from two to 65 months of age, freely available.
17The SWYC-BR was translated and adapted for Brazilian Portuguese and the validation revealed satisfactory measurement properties for the use in Brazil (Average Variance Extracted = 0.73 and Cronbach's Alpha = 0.97).
18 The tool is composed of 12 forms, one for each age group, containing ten items that should be fulfilled by the researcher from the answers of the children's parents or caregivers.
19This tool assesses multiples domains of child well-being: (1) Developmental Milestones (DM), which assesses cognitive, motor and language development; (2) Parent's concerns with behavior, learning or development of children; (3) Family questions, which assess the stress in family environment; (4) Baby Pediatric Symptom Checklist – BPSC and the Preschool Pediatric Symptom Checklist (PPSC), which assess behavioral and emotional symptoms of children under 18 months and between 18 and 65 months, respectively, and (5) Parent's observations of social interactions, which was not used in this study, since it is focused on children from 18 and 34 months.
18The dependent variable of the study was the risk of CD delay, classified as present or absent according to the cut-off point defined in the SWYC-BR for each age group. The independent variables were categorized into two groups: related to children (sex, ethnicity, age, birth weight, time of breastfeeding, time of hospitalization, sensitive condition and behavioral changes) and to the caregiver/environment (sex, ethnicity, schooling, marital status, number of children, religion, income, food insecurity, housing, sanitation and parental reading practices). We considered behavioral change when BPSC or PPSC presented scoring ≥ 3 in one of its subscales or ≥9, respectively.
18,19Behavioral changes were assessed as a quantitative nominal variable, described as "yes" or "no". The variables present in SWYC, related to parent's concerns with behavior, learning or development of children, were assessed with the Baby Pediatric Symptom Checklist – BPSC, divided into three subscales (inflexibility, irritability and difficulties with changes in routine). There is a risk of behavioral change when the sum of points of a subscale is ≥3. The Preschool Pediatric Symptom Checklist – PPSC assesses internalizing and externalizing behaviors, attentions problems and difficulties with routine, with risk of behavioral change when the sum of points is ≥9.
18,19Data were tabulated with double entry using Epi Info ™ software, version 3.5.1, for database validation, and subsequently exported to SPSS version 21.0 (SPSS Inc., Chicago, IL, USA) for statistical analysis. The variables were described in terms of absolute and relative frequency.
In order to identify variables associated with the risk of CD delay, we conducted a bivariate analysis using the Chi-square test or Fisher's exact test. The variables with statistical significance lower than or equal to 20% (
p<0.20) were selected for multivariate analysis, by means of Poisson regression with robust estimation and backward elimination method, in order to obtain the adjusted prevalence ratio estimates. The statistical significance was determined by the Wald test, with a 95% confidence interval and 5% significance level.
The study was approved by the Research and Ethics Committee of the Federal University of Pernambuco (CAAE: 52665821.2.0000.9430, Opinion number: 5.314.508).
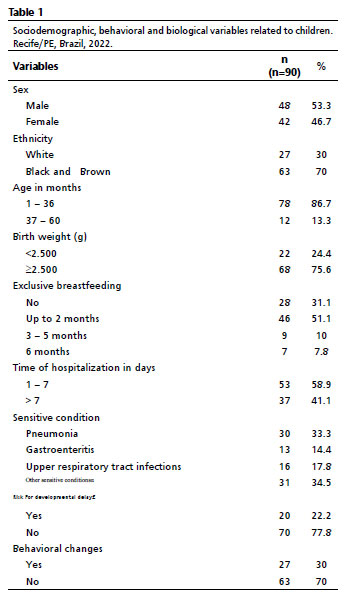
ResultsThe study included 90 children with PCSC and their respective caregivers. Most children were male (53.3%), black or brown (70%), had 36 months of age or less (86.7%) and had adequate birth weight (75.6%). The most frequent PCSCs were other sensitive conditions, such as anemia, asthma, vaccine-preventable diseases (34.5%) and pneumonia (33.3%). The risk of developmental delay was identified in 22.2% of children, and 30% showed behavioral changes (Table 1).
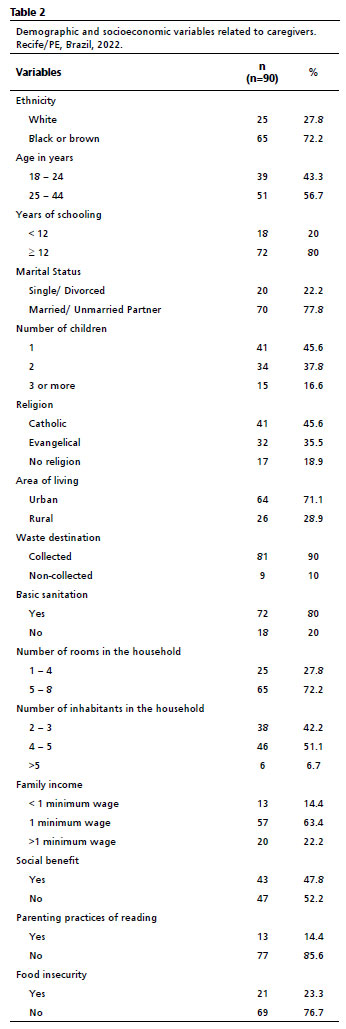
All caregivers were mothers of the children. Most of them self-declared as Black or Brown (72.2%), were aged between 25 and 44 years (56.7%) and had completed 12 or more years of schooling (80%). Most of them were married or cohabiting (77.8%). With regard to income, 63.4% of women had a family income of one minimum wage, and 52.2% did not receive social benefits. Most of them lived in areas with waste collection (90%), with access to basic sanitation (80%) (Table 2).
Table 3 presents results of the bivariate analysis for the variables related to children. We observed an association between the risk of developmental delay and birth weight <2500g (PR= 2.53; 95%CI= 1.21-5.30;
p=0.036) and the presence of behavioral changes (PR=3.5; 95% CI=1.62-7.59;
p=0.001).
Table 4 shows results of the bivariate analysis for the variables related to caregivers. We observed an association between the risk of developmental delay and the fact of caregivers having three or more children (PR=2.11, 95%CI=1.45-3.91;
p=0.025); residing in locations without basic sanitation (PR=3.27; 95%CI=1.60-6.68;
p=0.030), living with five people or more (PR=3.62; 95%CI=1.51-8.70,
p=0.038), and receiving any social benefit from the government (PR=2.55; 95%CI=1.07-6.04;
p=0.024).
Table 5 shows results of the bivariate analysis, which was initially conducted for the variables related to children. We identified an association between the risk of developmental delay and birth weight <2500g (PR=2.53; 95%CI=1.21-5.30;
p=0,036) and the presence of behavioral changes (PR=3.5; 95%CI=1.62-7.59;
p=0.001).
For the variables related to caregivers/environment, the analysis revealed associations between the risk of developmental delay and residing in locations without basic sanitation (PR=3.27; 95%CI= 1.60-6.68;
p=0.030), living in households with five or more people (PR=3.62; 95%CI=1.51-8.70;
p=0.038), having three or more children (PR=2.11; 95%CI=1.45-3.91;
p=0.025) and receiving social benefits (PR=2.55; 95%CI=1.07-6.04);
p=0.024).
The variables included in Poisson's regression model: birth weight, exclusive breastfeeding, behavioral changes, marital status, number of children, religion, area of residence, waste destination, basic sanitation, number of inhabitants and social benefit receipt.
After model adjustment, the risk of developmental delay was associated with factors such as the caregiver having two children (PR=1.18; 95%CI= 1.04-1.26;
p=0.032), residing in environments without basic sanitation (PR=1.19, 95%CI=1.03-1.37;
p=0.008), children with birth weight <2500g (PR=1.17; 95% CI=1.02-1.33;
p=0.026) and with behavioral changes (PR=1.14, 95%CI= 1.02-1.30;
p=0.037) (Table 5).
DiscussionFactors associated with developmental delay, identified by means of the SWYC-BR screening tool, in children hospitalized due to primary care-sensitive conditions were: low birth weight, behavioral changes, mothers with two children and residence in places without basic sanitation.
Among the main primary care-sensitive conditions (PCSC) found, we highlight pneumonia (33.3%) and gastroenteritis (14.4%), which reverberate the national data that evidenced the vulnerability of children under five years of age to health conditions such as gastroenteritis, pneumonia and asthma.
16Although we have not collected data on specific attributes of primary care, the frequency of children hospitalized due to PCSC indicates a potential association with child care accessibility, as observed in another study carried out in Minas Gerais. In this study, it was evidenced the relationship between these events and a potential impairment of child care in APS environment.
20The profile of children in the present study demonstrated a high percentage of children under three years of age who were Black or Brown and had been early weaned before two months of life. The data from our study indicate the influence of social determinants that affect issues related to health, disease, care, and risks associated with morbimortality and child development.
We also observed a high percentage of children with low birth weight. Besides the risk of developmental delay, low birth weight is associated with prematurity, with mortality in the beginning of life, and complications throughout childhood.
21 Children who were born with a weight lower than 2500 g presented higher risk of neonatal hospitalization and may present worse results in cognitive and motor development.
22Additionally, there is a correlation between the increase of hospitalizations of children with low birth weight and unfavorable socioeconomic status of their mothers.
21 The economic status of caregivers is an important factor, since living in locations without basic sanitation is often associated with a precarious socioeconomic status. Unhealthy environments represent an additional risk for cognitive and motor delay.
4The environment in which children live has a significant impact on their full development. Children in poverty contexts are more prone to experiencing negative effects on long-term brain and cognitive development.
23,24 For the caregiver, this economic condition results in the increase of parental stress and food insecurity.
3Parental stress is amplified by poverty
25 and the psychological suffering of parents may hinder adequate responses to adversities and to the interaction with children, impairing growth and development.
26 Food insecurity, generated by economic factors, contributes to childhood malnutrition, with consequences for growth, cognitive abilities and professional and educational performance.
27It is essential to invest in parental support actions for caregivers who experience high levels of stress, with the aim of encouraging responsive care and improving the caregiver-child interaction, even in adverse scenarios.
In the multivariate analysis, the risk of developmental delay was positively associated with variables such as: birth weight <2500g, having two children, living in a location without basic sanitation and children's behavioral changes. The association between number of children and risk of developmental delay was observed in a study that identified lower development scores in families with two or more children under seven years of age.
9 This finding may be explained by the division of attention and care, which are impaired when the family has more than one small child.
28Behavioral changes associated with the risk of developmental delay include inflexibility, irritability and difficulties with routine changes, besides problems of attention and internalizing and externalizing behaviors, particularly in hospitalized children, who challenge emotional vulnerabilities that are intensified by the hospital environment.
29Interventions based on positive parenting practices and responsive care may lead to significant benefits, and health professionals play an essential role in the guidance of caregivers and in the articulation between hospital and primary care.
30This study has important limitations, such as the cross-sectional design, which prevents causal relationships; the small sample size; and the absence of a control group with children not hospitalized due to PCSC. Although a direct association between hospitalizations due to PCSC and developmental delay was not identified, the results evidenced the influence of health social determinants in the integrative child care. These findings reinforce the importance of public policies that promote the development in early childhood and strengthen the Healthcare Network, focusing on the prevention of avoidable hospitalizations.
References1. Zhang L, Ssewanyana D, Martin MC, Lye S, Moran G, Abubakar A,
et al. Supporting child development through parenting interventions in low-to middle-income countries: an updated systematic review. Front Public Health. 2021; 9: 671988.
2. Ilyka D, Johnson MH, Lloyd-Fox S. Infant social interactions and brain development: A systematic review. Neurosci Biobehav Rev. 2021;130: 448-69.
3. Black MM, Walker SP, Fernald LC, Andersen CT, DiGirolamo AM, Lu C,
et al. Early childhood development coming of age: science through the life course. Lancet. 2017; 389 (10064): 77-90.
4. Gil JD, Ewerling F, Ferreira LZ, Barros AJ. Early childhood suspected developmental delay in 63 low-and middle-income countries: Large within-and between-country inequalities documented using national health surveys. J Global Health. 2020; 10 (1): 010427.
5. Ministério da Saúde (BR). Fundação Maria Cecilia Souto Vidigal. Resumo Executivo Projeto PIPAS 2022: Indicadores de desenvolvimento infantil integral nas capitais brasileiras. Brasília (DF): Ministério da Saúde; 2023. [access in 2024 Out 07]. Available from:
http://bvsms.saude.gov.br/bvs/publicacoes/projeto_pipas_2022_resumo_executivo.pdf 6. Sania A, Sudfeld CR, Danaei G, Fink G, McCoy DC, Zhu Z,
et al. Early life risk factors of motor, cognitive and language development: a pooled analysis of studies from low/middle-income countries. BMJ open. 2019; 9 (10): e026449.
7. Araujo WRM, Malta MB, Faggiani LD, Cardoso MA, Matijasevich A, MINA‐Brazil Study Group. Suspected neuropsychomotor developmental delay in the first 2 years of life in a birth cohort in the Brazilian Amazon: Incidence, persistence and risk factors. Infant Child Dev. 2022; 31 (2): e2287.
8. Dias TL, Moraes AR, Brito TM, Motta AB, Enumo SRF. Estresse da hospitalização e seu enfrentamento em crianças. Mundo Saúde. 2022; 46: 551-62.
9. Lehner DC, Sadler LS. Toddler developmental delays after extensive hospitalization: primary care practitioner guidelines. Paediatr Nurs. 2015; 41 (5): 236-42.
10. Pinto Junior EP, Aquino R, Dourado I, Costa LDQ, Silva MGC. Internações por condições sensíveis à Atenção Primária à Saúde em crianças menores de 1 ano no Brasil. Ciên Saúde Colet. 2020; 25: 2883-90.
11. World Health Organizantion (WHO). Newborn death and illness. The Partnership: for Maternal, Newborn & Child Health [
Internet]. 2011 [access in 2020 Jun 15]. Available from:
http://www.who.int/pmnch/media/press_materials/fs/fs_newborndealth_illness/en/12. Souza JM, Veríssimo MLOR. Desenvolvimento infantil: análise de um novo conceito. Rev Latino-Am Enferm. 2015; 23 (6):1097-104.
13. Buss PM, Pellegrini Filho A. A saúde e seus determinantes sociais. Physis. 2007; 17 (1): 77-93.
14. Atashbahar O, Sari AA, Takian A, Olyaeemanesh A, Mohamadi, E, Sayye Barakati SH. The impact of social determinants of health on early childhood development: a qualitative context analysis in Iran. BMC Public Health 2022; 22 (1): 1-13.
15. Amaral JV, Brito VS, Araújo Filho ACA, Brito MA, Dantas ALB, Rocha SS. Cuidado do enfermeiro na prevenção de hospitalizações infantis por condições sensíveis à atenção primária. Rev Soc Bras Enferm Ped. 2021; 21 (2): 110-8.
16. Prezotto KH, Chaves MMN, Mathias TAF. Hospitalizações sensíveis à atenção primária em crianças, segundo grupos etários e regionais de saúde. Rev Esc Enferm USP. 2015; 49 (1): 44-53.
17. Guimarães MAP, Magalhães LDC, Moreira RS, Bessa FR, Alves CRL. Preliminary Norms for Screening for Developmental Delay in Brazilian Children Younger than 65 Months. J Dev Behav Pediatr. 2022; 43 (9): e614-22.
18. Moreira RS, Magalhães LC, Siqueira CM, Alves CRL. Cross-cultural adaptation of the child development surveillance instrument "Survey of Wellbeing of Young Children (SWYC)" in the Brazilian context. J Hum Growth Dev. 2019; 29 (1): 28-38.
19. Alves CRL, Guimarães MAP, Moreira RS. Survey of Well-being of Young Children (SWYC-BR): manual de aplicação e interpretação [
Internet]. 2
nd ed. Araranguá: UFSC; 2022 [access in 2023 Jul 19]. Available from:
https://repositorio.ufsc.br/bitstream/handle/123456789/220345/Manual%20do%20SWYC-Br.pdf?sequence=320. Leão HM, Caldeira AP. Acessibilidade e trajetórias de cuidado para crianças com internações por condições sensíveis à atenção primária. Ciênc Saúde Colet. 2021; 26 (8): 3301-10.
21. Quaresma ME, Almeida AC, Méio MDB, Lopes JMA, Peixoto MVM. Fatores associados a internação durante o período neonatal. J Pediatr. 2018; 94: 390-8.
22. Xu Y, Guo X, Pan Z, Zheng G, Li X, Qi T,
et al. Perinatal risks of neonatal and infant mortalities in a sub-provincial region of China: a livebirth population-based cohort study. BMC Pregnancy Childbirth. 2022; 22 (1): 338.
23. Pérez-Pereira M, Fernández MP, Gómez-Taibo ML, Martínez-López Z, Arce C. A follow-up study of cognitive development in low risk preterm children. Int J Environ Res Public Health. 2020 Mar; 17 (7): 2380.
24. Judd N, Sauce B, Wiedenhoeft J, Tromp J, Chaarani B, Schliep A,
et al. Cognitive and brain development is independently influenced by socioeconomic status and polygenic scores for educational attainment. Proc Natl Acad Sci USA. 2020 Jun; 117 (22): 12411-8.
25. Miller GE, Culhane J, Grobman W, Simhan H, Williamson DE, Adam EK,
et al. Mothers' childhood hardship forecasts adverse pregnancy outcomes: role of inflammatory, lifestyle, and psychosocial pathways. Brain Behav Immun. 2017; 65: 11-9.
26. Silva IDCPD, Cunha KDC, Ramos EMLS, Pontes FAR, Silva SSDC. Estresse parental em famílias pobres. Psicol Estud. 2019; 24: e40285.
27. Chaudry A, Wimer C. Poverty is not just an indicator: the relationship between income, poverty, and child well-being. Acad Pediatr. 2016; 16 (3): 23-9.
28. UNICEF. Breastfeeding. Unicef data: Monitoring the situation of children and women. 2022. [
Internet]. [access in 2022 Oct 09]. Available from:
https://data.unicef.org/topic/nutrition/breastfeeding/29. Kodish I. Behavioral Health Care for Children Who Are Medically Hospitalized. Pediatr Ann. 2018; 47 (8): e323-7.
30. Black MM, Behrman JR, Daelmans B, Prado EL, Richter L, Tomlinson M,
et al. The principles of Nurturing Care promote human capital and mitigate adversities from preconception through adolescence. BMJ Glob Health. 2021; 6 (4): e004436.
Authors' contribution: Carvalho JS: conceptualization, data curation, data collection, data analysis, writing, review and editing of the manuscript; de Paula WKA, Coriolano-Marinus MWL: conceptualization, data curation, data collection, data analysis, supervision, writing, review and editing of the manuscript; Lima APE, Leal LP: data analysis, writing, review and editing of the manuscript. All authors approve the final version of the article and declare no conflicts of interest.
Data Availability: The entire data set supporting the results of this study has been published in the article itself.
Received on June 6, 2024
Final version presented on March 24, 2025
Approved on May 6, 2025
Associated Editor: Karla Bomfim
 ; Weslla Karla Albuquerque de Paula2
; Weslla Karla Albuquerque de Paula2 ; Ana Paula Esmeraldo Lima3
; Ana Paula Esmeraldo Lima3 ; Luciana Pedrosa Leal4
; Luciana Pedrosa Leal4 ; Maria Wanderleya de Lavor Coriolano Marinus5
; Maria Wanderleya de Lavor Coriolano Marinus5