ABSTRACT
OBJECTIVES: to investigate predictors of emotional and behavioral difficulties in a sample of adolescents from São Leopoldo/RS.
METHODS: longitudinal study that followed children from birth to 13 years of age. Sociodemographic, maternal and perinatal variables were obtained at six months and from 12 to 16 months, anthropometric variables and screen time at four and eight years. At age 13, 174 adolescents completed the Strengths and Difficulties Questionnaire (SDQ).
RESULTS: In the total SDQ assessment, 14.4% presented emotional and behavioral difficulties. In the subscales, we observed: increased changes in conduct among children of mothers with <8 years of schooling (p=0.028); adolescents born to mothers <20 years old showed an increase in emotional changes (p=0.043); greater difficulties in prosocial behavior in male adolescents (p=0.019), white (p=0.049), exclusively breastfed for <4 months (p=0.036), families with monthly income <3 minimum wages (p=0.005) and had a higher mean BMI z-score at four years of age (p=0.003).
CONCLUSION: Shorter breastfeeding time, excess child weight, young age and low maternal schooling and low socioeconomic conditions were predictors of the outcome, which reinforces the importance of multidisciplinary prevention actions in child and adolescent mental health.
Keywords:
Adolescent, Breastfeeding, Obesity, Psychosocial functioning, Mental health
RESUMO
OBJETIVOS: investigar preditores de dificuldades emocionais e comportamentais numa amostra de adolescentes de São Leopoldo/RS.
MÉTODOS: estudo longitudinal que acompanhou crianças do nascimento aos 13 anos de idade.Variáveis sociodemográficas, maternas e perinatais foram obtidas aos seis meses e dos 12 aos 16 meses,variáveis antropométricas e o tempo de tela aos quatro e oito anos. Aos 13 anos, 174 adolescentes completaram o Strengths and Difficulties Questionnaire (SDQ).
RESULTADOS: na avaliação total do SDQ, 14,4% apresentaram dificuldades emocionais e comportamentais. Nas subescalas, observamos: aumento de alterações de conduta entre filhos de mães com escolaridade <8 anos (p= 0,028); adolescentes filhos de mães com <20 anos apresentaram aumento de alterações emocionais (p=0,043); maiores dificuldades no comportamento pró-social nos adolescentes masculinos (p= 0,019), cor branca (p=0,049), amamentados exclusivamente por <4 meses (p=0,036), famílias com renda mensal <3 salários mínimos (p=0,005) e apresentavam maior média de z-score do IMC aos quatro anos de idade (p=0,003).
CONCLUSÃO: o menor tempo de aleitamento materno, o excesso de peso infantil, a pouca idade e baixa escolaridade materna e baixas condições socioeconômicas foram preditores do desfecho, o que reforça a importância de ações multidisciplinares de prevenção em saúde mental infantojuvenil.
Palavras-chave:
Adolescente, Aleitamento materno, Obesidade, Funcionamento psicossocial, Saúde mental
IntroductionChildren and adolescents' mental health has received greater attention over the last few decades due to the increasingly early onset of mental health disorders (MHO) and, even if some diseases go into remission, many will continue to have MHO in adulthood, generating negative short- and long-term consequences for the functioning of these individuals, with a heavy personal, family and socioeconomic burden.
1Biopsychosocial integration allows humans to adapt to the environment, but throughout the life cycle, especially in adolescence - a phase of intense physical, cognitive, social and emotional changes - risk factors for MHO can arise. These factors can be biological, psychological, familial, cultural and environmental, ranging from the individual and community level to the wider social context.
1,2 In underdeveloped countries, socioeconomic aspects such as low income, low schooling, social exclusion and violence are relevant predictors of MHO, although no single factor has a high predictive value.
3,4Exposure to a single risk factor in childhood and adolescence generally has little impact, but the sum of multiple factors increases the vulnerability.
4 However, protective factors can counteract adverse effects, influencing long-term psychosocial development. The prevalence of MHO is high globally and as in Brazil, affecting around 10% of the children throughout their lives.
1,3Given this relevance, this study aims to investigate predictors of emotional and behavioral difficulties in adolescents from São Leopoldo (RS), helping to broaden the literature scope on the subject.
MethodsThis is an analysis of secondary data from a longitudinal database
5 with an initial base of data collected from children at birth, at the
Hospital Centenário, in the city of São Leopoldo, Rio Grande do Sul/Brazil, and these children were followed up from then until the age of 13. The anchor study was conducted in four phases of data collection, through home interviews with the mothers/children: the first was when the children were between 12 and 16 months old, the second was at age of four, the third at eight years old and the fourth in adolescence, at 13.
The analyses in this study are longitudinal, since the intervention was carried out in the anchor study there were no impact on the outcomes assessed.
In this study, the sample size was calculated using the WinPEPI program (Programs for Epidemiologists for Windows), version 11.43, based on a pilot study with 20 adolescents, due to the scarcity of data in the literature. Considering a significance level of 5%, statistical power of 85% and a minimum effect size of 0.47 standard deviations between the groups, a minimum total number of 156 adolescents was obtained for the variables "breastfeeding", "body mass index" and "screen time".
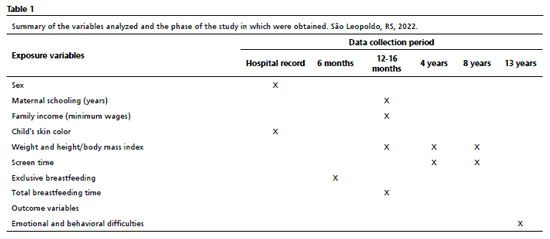
Table 1 summarizes the variables used and at which stage of the study they were obtained. Information on the children's sex and race, maternal and breastfeeding information, anthropometric variables and screen time were obtained from the anchor study. Sex and race were obtained from the children's hospital records at birth and maternal information was obtained from 12 to 16 months through structured face-to-face interviews with the mothers: maternal schooling, occupation, maternal age at birth and family income. In the interviews at six months and 12 to 16 months, the mothers were asked about breastfeeding. We considered exclusive breastfeeding when it was the only food offered to the child, without offering tea or water. In turn, breastfeeding was defined as the presence of breastmilk in the child's diet, regardless of any other food being offered.
With regard to anthropometric variables, from 12 to 16 months of age, the children's weight was measured using a portable digital scale (Techline, São Paulo, Brazil). Length was measured using an infant stadiometer (Serwital Inc., Porto Alegre, Brazil). At four, eight and 13 years of age, the children were weighed in light clothing, without shoes, on a digital scale (Techline, São Paulo, Brazil), and standing height was measured to the nearest 0.1 cm using a stadiometer (SECA, Hamburg, Germany). All measurements were converted into body mass index (BMI) z-scores by age, based on the World Health Organization
6 growth standards, where a z-score greater than +1 was considered overweight.
The interviews that took place on the children's fourth and eighth years of age, questions were asked about the number of hours spent watching television, in front of the computer, video games and cell phones. This period was added up and considered as screen exposure time.
The instrument used to assess the outcome of the current study was the Strengths and Difficulties Questionnaire (SDQ), adolescent version, developed by Goodman
7 in the 1990s and validated in Brazil by Fleitlich-Bylik
et al.,
8 which was answered by the adolescents taking part in the study themselves, using the extended version of the SDQ intended for adolescents aged between 11 and 16, applied individually, in anonymous self-completion mode.
The SDQ instrument, which is an MHO screening tool, investigates symptoms of emotional and behavioral difficulties and abilities in children and adolescents and their impact on their family and school experiences.
7 It consists of 25 items, grouped into five subscales that assess: hyperactivity, emotional alterations, conduct alterations, alterations in relationships with peers and pro-social behavior.
7 Of the five subscales, four track behavioral changes and, together, provide the total of the child and adolescent's difficulties and the fifth deals with a competence, pro-social behavior.
7Each SDQ subscale has five items, where the answers can be: false, somewhat true or true, and each item receives a specific score; the score of each subscale is obtained by adding up the scores of the items, which can range from zero to ten (Table 2).
7 On the total difficulties scale, higher scores represent more difficulties (possible scores from zero to 40) and on the pro-social behavior scale, higher scores represent more favorable pro-social behavior (possible scores from zero to ten); the sum of each scale and the total sum allows the adolescent to be classified into three categories: development without difficulties, borderline or with emotional and behavioral difficulties (Table 3).
7 According to the cut-off scores adopted by Goodman
7, children and adolescents with total scores between zero and 13 are defined as having no difficulties, scores between 14 and 16 are considered borderline and scores between 17 and 40 are considered to have emotional and behavioral difficulties in the SDQ assessments. For the subscale scores, the following cut-off values were applied: emotional alterations: 0-3 = no alterations, 4 = borderline, 5-10 = with alterations; conduct alterations: 0-2 = no alterations, 3 = borderline, 4-10 = with alterations; hyperactivity / inattention: 0-5 = no changes, 6 = borderline, 7-10 = with changes; changes in relationships with peers: 0-2 = no changes, 3 = borderline, 4-10 = with changes; and pro-social behavior: 6-10 = no changes, 5 = borderline, 0-4 = with changes (Table 3).
The study analyzed MHO screening in the community sub-sample of adolescents from the anchor project who were considered to be at low risk. To assess the outcome, only the emotional and behavioral difficulties category was used, considering the individual sum of each subscale and the total of the SDQ subscales.
7,8The study by Vugteveen
et al.
9 demonstrated the invariance of the SDQ measurement between clinical and community populations, ensuring that the community-focused analysis did not disregard potential setting effects.
The SDQ is widely recognized for its reliability and is widely used in international research. Available in a variety of languages, it is applied both in the clinical context, to measure symptoms and/or psychopathological impacts, and in community studies, to screen for MHO in children and adolescents.
9,10,11Data processing and analysis were conducted in the SPSS Statistics for Windows program, version 19.0 (USA). For statistical analysis, we calculated the frequencies of categorical variables, the means and standard deviation of symmetrical continuous variables, and the medians and interquartile ranges of asymmetrical continuous variables. The Mann-Whitney association test was used to check for differences between the parametric continuous variables between the groups classified according to the results of the SDQ questionnaire. The chi-square test was used to check for possible associations between categorical variables, where the level of statistical significance considered was
p<0.05.
This study was approved by the Human Research Ethics Committee of the
Universidade do Vale do Rio dos Sinos -UNISINOS, São Leopoldo/RS, under Opinion N
o. 407.263.
ResultsThe current study showed a higher mean BMI z-score at four years of age among adolescents who showed changes in pro-social behavior (1.20
vs. 0.16;
p=0.003) (Table 4).
The study found that adolescents with scores for emotional and behavioral alterations on the total SDQ scale had a higher mean BMI z-score at four and eight years of age (
p=0.047 and
p=0.015, respectively) (Table 5).
Each subscale was analyzed separately in relation to the independent variables, and the results are presented separately below:
Conduct disorders: there was a higher prevalence of conduct disorders among the children of mothers with less than eight years of schooling (
p=0.028) (Table 5).
Emotional alterations: adolescents born to mothers aged under 20 at the time of their birth had a higher prevalence of emotional alterations (23.1%
vs. 8.8%;
p=0.043) (Table 5).
Pro-social behavior: there was a higher prevalence of alterations in the pro-social behavior subscale among adolescents who were male (
p=0.019), had white skin (
p=0.049), were exclusively breastfed for less than four months (
p=0.038), and belonged to families with a monthly income of less than three minimum wages (
p=0.005). The fact that the mother worked out of home was identified as an association trend for changes in pro-social behavior among adolescents (
p=0.058) (Table 5).
The subscales for changes in peer relationships and changes in hyperactivity were not associated with the independent variables studied.
DiscussionThe important contributions in this study include the identification of variables that predict emotional and behavioral difficulties in adolescence, indicating a shorter period of breastfeeding, being overweight at the age of four, low maternal schooling, young age and low family socioeconomic conditions as predictors of this risk.
The importance of breastfeeding is widely justified due to its nutritional, cognitive and psychosocial benefits. However, few studies have analyzed its effects in adolescence and adulthood.
12,13,14 The findings of this study reinforce the importance of public policies to promote and encourage exclusive breastfeeding for up to six months.
15,16 In addition, adolescents who were exclusively breastfed for less than four months performed worse on the pro-social behavior subscale.As social skills and peer relationships have a strong impact on neuropsychic development, their absence can increase the risk of MHO.
17The associations between behavioral changes and socioeconomic and maternal factors found in this study corroborated the results published in a study conducted in the United Kingdom with adolescents, which showed an inverse relationship between socioeconomic status and MHO at the age of 14. Low maternal schooling, especially in early childhood, increased the risk of MHO in adolescence by up to four times.
18 A review by Vilhena and Paula
19 highlighted low maternal schooling as a significant risk factor for conducting disorders in adolescence. The findings reinforce the necessity for governmental and non-governmental efforts to promote economic, educational and social development in Brazil, with a view to reducing inequalities and their negative impact on MHO.
Early pregnancy, before the age of 20, has various repercussions, although the study by Monteiro
et al.
20 shows a decrease in the percentage of teenage mothers from 23.4% (2000) to 14.7% (2019). Despite publications in the area, few studies have monitored the mental health of children during adolescence. Unlike a study by Monteiro
et al.,
21 from São Paulo, which identified an increase in internalizing alterations, this study revealed that children of adolescent mothers showed more emotional alterations in the SDQ, but no association with difficulties in peer relationships. These findings may be linked to other gestational factors related to MHO.
22Childhood obesity is considered one of the world's major public health problems.
6 The mental health of children with obesity has been gaining ground in the literature, as MHO generally acts as a maintainer and hinders the success of childhood obesity treatments.
23 Previous publications have concluded that childhood obesity has psychosocial consequences for the lives of these individuals and can compromise not only their physical health, but also their psychological health and quality of life, with repercussions in adulthood.
6,24,25This study found a higher mean BMI z-score at the age of four among adolescents who showed changes in pro-social behavior and, in addition, those adolescents with a score of changes in the total SDQ scale had a higher mean BMI z-score at four and eight years of age (
p=0.047 and
p=0.015), respectively, as shown in other studies.
26,27 The results point to emotional difficulties in children with a higher BMI and highlight the importance of including psychological screening in the treatment of overweight children.
The
Sociedade Brasileira de Pediatria28 (Brazilian Society of Pediatrics) warns that the early and excessive use of digital technologies in children can have a negative impact on attention, patience and control of impulsivity, as well as contributing to hyperactivity and low frustration tolerance. In this context, we observed that adolescents with greater changes in the hyperactivity subscale had a higher average screen time in preschool and childhood school (3.4h
vs. 2.5h), suggesting a trend of statistical significance.
The main strength of the study is the psychometric capacity of the SDQ to screen for MHO in adolescents, reducing classification bias. However, a limitation is a selection of bias, since the sample was made up of patients treated at a maternity hospital linked to
Sistema Único de Saúde (SUS) (Public Health System). In addition, the use of a secondary database may have introduced temporal limitations, such as the impact of MHOs related to the COVID-19 pandemic.
29It is also important to consider that other individual, family and social factors that have not been evaluated and may influence childhood and adolescent's MHO, such as a history of domestic violence, abuse, genetic factors, educational context, social assistance and access to health services.
30We conclude that the results found provide evidence that reinforces the importance of planning early and preventive multidisciplinary and intersectoral actions to assertively tackle an issue as complex as childhood MHOs. It is suggested that new Brazilian studies be encouraged to help better understand the prevalent scenario of childhood MHOs, as well as their long-term impact based on longitudinal studies.
References1. Gobel K, Cohrdes C. The whole is greater than the sum of its parts: profiles of multiple mental health risk factors using Latent class analysis. Child Adolesc Psychiatry Ment Health. 2021; 15 (1): 27.
2. Oliveira WA, Gea B, Marcon GH, Oliveira JL, Dalpino LR, Freire TN,
et al. Perception of professionals on the social determinants of child and adolescent mental health. Quaderns Psicol. 2022; 24 (1): e1654.
3. Kieling C, Buchweitz C, Caye A, Silvani J, Ameis SH, Brunoni AR,
et al. Worldwide prevalence and Disability from mental disorders across childhood and adolescence.
JAMA Psychiatry. 2024; 81 (4): 347-56.
4. García CR, Villarejo CB, Villardón GL. Children and adolescents mental health: a systematic review of interactionbased interventions in schools and communities. Frontiers Psychol. 2019; 10: 918.
5. Ferreira RC, Marin AH, Vitolo MR, Campagnolo PDB. Early ultra-processed foods consumption and hyperactivity/inattention in adolescence. Rev Saúde Pública. 2024; 58 (1): 46.
6. WHO Multicentre Growth Reference Study Group (WHO). Child Growth Standards based on length/height, weight and age. Acta Paediatr 2006; 450 (Suppl.): 76-85.
7. Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry. 1997; 38 (5): 581-6.
8. Fleitlich B, Cortázar PG, Goodman R. Skills and Difficulties Questionnaire (SDQ). Rev Neuropsychiatr Childhood. 2000; 8 (1): 44-50.
9. Vugteveen J, Bildt A de, Serra M, Wolff MS, Timmerman ME.Psychometric properties of the dutch strengths and difficulties questionnaire (SDQ) in adolescent community and clinical populations. Assessment. 2020; 27 (7): 1476-89.
10. Vugteveen J, de Bildt A, Theunissen M, Reijneveld SA, Timmerman M. Validity aspects of the strengths and difficulties questionnaire (SDQ) adolescent self-report and parent-report versions among dutch adolescents. Assessment. 2021; 28 (2): 601-16.
11. Theunissen M, Wolff MS, Reijneveld SA. The Strengths and Difficulties Questionnaire Self-Report: A Valid Instrument for the Identification of Emotional and Behavioral Problems. Acadpediatr. 2019; 19 (4): 471-6.
12. Soled D, Keim SA, Rapoport E, Rosen L, Adesman A. Breastfeeding Is Associated with a Reduced Risk of Attention-Deficit/Hyperactivity Disorder Among Preschool Children. J Dev Behav Pediatr. 2021; 42 (1): 9-15.
13. Zeng Y, Tang Y, Tang J, Shi J, Zhang L, Zhu T,
et al. Association between the different duration of breastfeeding and attention deficit/hyperactivity disorder in children: a systematic review and meta-analysis. Nutr Neurosci. 2020; 23 (10): 811-23.
14. Girard LC, Farkas C. Breastfeeding and behavioural problems: Propensity score matching with a national cohort of infants in Chile. BMJ Open. 2019; 9 (2): e025058.
15. Almeida CR, Coutinho ESF, Silva DA, Oliveira ERA, Bloch KV, Viana MC. Exposição ao aleitamento materno e transtornos mentais comuns na adolescência. Cad Saúde Pública. 2019; 35 (5): e00093718.
16. Fava DC, Andretta I, Marin AH. Emotional and Behavior problems in children: associated and predictive factors. Rev Bras Ter Cogn. 2023; 19 (1): 61-9.
17. Lehmkuhl L, Arakawa-Belaunde A. Fatores de risco e proteção para a saúde mental na adolescência em cidades pequenas. RBM. 2021; 24 (3): 155-77.
18. Straatmann VS, Lai E, Lange T, Campbell MC, Wickham S, Andersen AN,
et al. How do early life factors explain social inequalities in adolescent mental health? Findings from the UK Millennium Cohort Study. J Epidemiol Community Health. 2019; 73 (11): 1049-60.
19. Vilhena K, Paula CS. Problemas de conduta: prevalência, fatores de risco/proteção: impacto na vida escolar e adulta. Cad Pós-Grad Distúrb Desenvolv. 2017; 17 (1): 39-52.
20. Oliveira-Monteiro NR de, Freitas JV, Aznar-Farias M. Transcorrer da gravidez na adolescência: Estudo longitudinal quando os filhos são adolescentes. Psicol Estud. 2014; 19 (4): 669-79.
21. Monteiro DLM, Monteiro IP, Machado MSC, Bruno ZV, Silveira FA, Rehme MFB,
et al. Trends in teenage pregnancy in Brazil in the last 20 years (2000-2019). Rev Assoc Med Bras. 2021; 67 (5): 759-65.
22. Silva BM, Nogueira BRV, Lopes GS, Souza LR, Barros NPS, Freitas RA,
et al. Fatores de risco associados à gravidez na adolescência: revisão integrativa. Res Soc Dev. 2020; 9 (11): e39691110109.
23. Sagar R, Gupta T. Psychological Aspects of Obesity in Children and Adolescents. Indian J Pediatr. 2018; 85 (7): 554-9.
24. Förster LJ, Vogel M, Stein R, Hilbert A, Breinker JL, Böttcher M,
et al. Mental health in children and adolescents with overweight or obesity. BMC Public Health. 2023; 23 (1): 135.
25. Carsley S, Pope E, Tu K, Parkin PC, Toulany A, Birken CS. Association between Weight Status and Mental Health Service Utilization in Children and Adolescents. J Can Acad Child Adolesc Psychiatry. 2020; 29(4): 229-40.
26. Vanvuuren CL, Watcher GG, Veenstra R, Rijnhart JJM, Vanderwal MF, Chinapaw MJM,
et al. Associations between overweight and mental health problems among adolescents, and the mediating role of victimization. BMC Public Health. 2019; 19: 612.
27. Bacchini D, Licenziati MR, Affuso G, Garrasi A, Corciulo N, Driul D,
et al. The interaction between BMI z-score, peer victimization and self-concept in overweight or obese outpatient children and adolescents. Childhood Obes. 2017; 13 (3): 242-9.
28. Sociedade Brasileira de Pediatria. Grupo de Trabalho Saúde na Era Digital (2022-2024). Manual de orientação: Menos tela, mais saúde. [
Internet]. 2024. [access in 2024 Set 3]. 163: 1-15. Available from:
https://www.sbp.com.br>departamentos>saude-digital#Menos Telas#Mais Saúde-Atualização 2024.
29. Figueiredo CS, Sandre PC, Portugal LCL, Mázala OT, Silva CL, Raony Í,
et al. COVID-19 pandemic impact on children and adolescents' mental health: Biological, environmental, and social factors. Prog Neuropsychopharmacol Biol Psychiatry. 2021; 106:110171.
30. Lund BS, Carrie B, Florence BEC, Breuer E, Chandra P, Haushofer J,
et al. Social determinants of mental disorders and the Sustainable Development Goals: a systematic review of reviews. Lancet Psychiatry. 2018; 5 (4): 357-69.
Acknowledgments: We would like to thank the
Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (National Council for Scientific and Technological Development) and the
Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul Rio Grande do Sul (FAPERGS) (Research Foundation) for their financial support.
Authors' contribution: Rosário KO: data analysis, writing and revision of the manuscript. Dal Bó Campagnolo P: data analysis and revision of the manuscript. All the authors have approved the final version of the article and declare no conflict of interest.
Received on September 2, 2024
Final version presented on April 2, 2025
Approved on April 4, 2025
Associated Editor: Ana Albuquerque
 ; Paula Dal Bó Campagnolo2
; Paula Dal Bó Campagnolo2